The Hidden Toll of Menopause Symptoms
Picture this: It’s 7 a.m. on a Tuesday, and Sarah, a 48-year-old marketing director, jolts awake drenched in sweat, her heart racing like she’s just run a marathon. She glances at the clock, knowing she’ll barely make it to her morning meeting without another wave crashing over her. The fan on her nightstand is already whirring, but it’s no match for the heat radiating from within. This isn’t a nightmare—it’s menopause, and for millions of women like Sarah, it’s rewriting their daily scripts in ways no one prepared them for.
Menopause isn’t just a milestone; it’s a seismic shift.
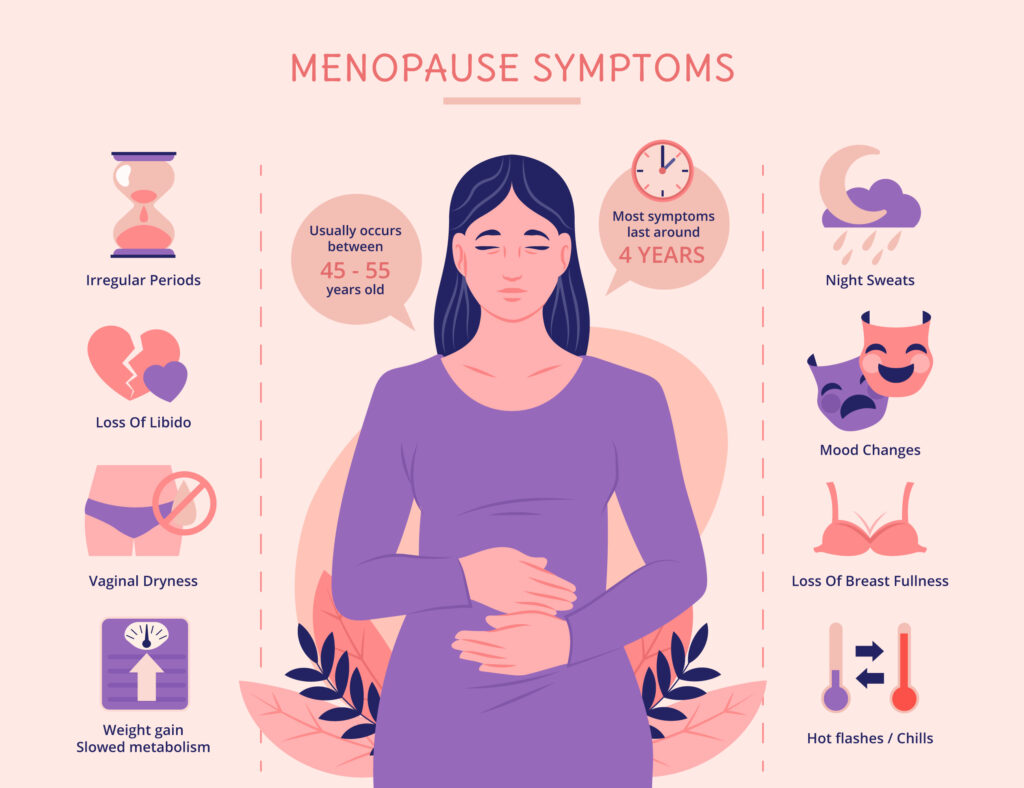
Defined by the World Health Organization as the permanent end of menstrual cycles due to the ovaries’ fading follicular function, it typically hits between ages 45 and 55, though symptoms can sneak in a decade earlier. By 2025, over a billion women globally are navigating this phase, yet conversations still feel hushed, like an embarrassing family secret.
The result? A silent epidemic of symptoms that chip away at energy, focus, and joy, often dismissed as “just aging.” But make no mistake: These changes are real, measurable, and profoundly disruptive, and women deserve to understand what’s happening to their bodies. Let’s start with the heavy hitters: vasomotor symptoms, better known as hot flashes and night sweats. These aren’t your grandma’s “power surges”—they’re brutal, unpredictable, and affect up to 80% of women going through menopause. Imagine your internal thermostat gone haywire, spiking your body temperature by a full degree in seconds, leaving you flushed, clammy, and desperate for a fan—or an ice bath. A 2025 study in The Lancet Diabetes & Endocrinology tracked symptom prevalence across the transition and found hot flushes jumping from a modest 8.8% in premenopause to a staggering 45-60% during perimenopause, with severity peaking for many in their late 40s.
For about 25% of sufferers, these episodes strike 10 or more times a day, lasting up to 30 minutes each, disrupting everything from boardroom presentations to bedtime routines. For women like Maria, a 50-year-old nurse, it’s not just the heat—it’s the embarrassment of visibly sweating through a patient consult, forcing her to carry spare blouses to work. But the heat isn’t the only thief in the night. Sleep disturbances tag along for 40-60% of women, turning rest into a battleground. Night sweats wake you every couple of hours, leaving sheets soaked and your mind foggy by dawn. The Bonafide Health’s 2025 State of Menopause survey, polling over 2,000 U.S. women aged 40-64, revealed that 62% reported chronic insomnia tied directly to these symptoms, with perimenopausal women hit hardest—many describing it as feeling like “living in a steam room you can’t escape.”
This isn’t hyperbole; poor sleep cascades into daytime fatigue, impairing concentration and decision-making. One respondent in the survey likened it to “parenting a newborn, but without the baby or the break.” Add to that the frustration of tossing and turning while your partner sleeps soundly, and it’s no wonder 35% of women report strained relationships due to sleep disruptions.Mood swings and brain fog add another layer of chaos. Hormonal dips in estrogen don’t just mess with your body—they hijack your headspace. Up to 50% of menopausal women grapple with anxiety or depression, a spike that’s often underreported because, well, who wants to admit they’re unraveling over spilled coffee? The same Bonafide report found 47% of participants experiencing “moderate to severe” emotional turbulence, with irritability leading the pack at 55%.
For someone like Priya, a 46-year-old accountant, the sudden tears during a routine budget meeting were as baffling as they were mortifying. And cognitive glitches? Forgetfulness, word-finding struggles—these affect 35-40% and can tank professional confidence. A University of Virginia study from early 2025 shocked researchers by showing 55.4% of women aged 30-35 already reporting moderate-to-severe symptoms on the Menopause Rating Scale, suggesting the “transition” starts way sooner than we thought. This early onset, dubbed “pre-perimenopause,” is flipping the script on when women should start preparing.
Joint aches plague 40%, mimicking arthritis, while weight gain—averaging 5-10 pounds around the midsection—stems from metabolic slowdowns. These aren’t vanity issues; they’re barriers to movement and self-esteem. Take Rachel, a 49-year-old yoga instructor, who noticed her once-fluid poses now triggered knee pain, forcing her to modify classes and grapple with a new sense of limitation. Add in hair thinning, reported by 20-30% of women due to hormonal shifts, and the mirror becomes another battleground.
The ripple effects on daily life are profound. At work, hot flashes correlate with a 10-15% dip in productivity, per a 2025 analysis, as women juggle symptom management with deadlines. For women in high-stakes roles, like Sarah navigating corporate pitches, the fear of a mid-meeting flush can erode confidence.
Relationships suffer too—partners report feeling sidelined, with 30% of surveyed couples noting increased tension from sleep disruptions alone. The emotional distance can grow when intimacy takes a hit, as partners struggle to understand the changes. And the economic hit? Untreated symptoms cost the U.S. economy $26 billion yearly in lost wages and healthcare, a figure likely climbing as our population ages. Globally, the impact is even starker, with low-resource regions lacking access to basic menopause education, leaving women to navigate this alone.Yet, amid this, there’s a silver lining emerging in 2025: Awareness is flipping the script. Women are demanding better—joining online forums, pushing for workplace accommodations like flexible hours or cooling stations, and educating themselves on the science.
Take Lisa, a 52-year-old teacher from Ohio, who after years of suffering in silence, started a local support group. “It was like finally naming the monster,” she says. Studies back this up; early education reduces symptom severity by 20-30% by empowering proactive steps. Social media platforms like X are buzzing with menopause advocates sharing tips, from cooling pillowcases to herbal teas, creating a virtual sisterhood that’s breaking the stigma. In fact, a 2025 survey found 65% of women felt more empowered after connecting with others online. So, what can you do if you’re nodding along, feeling Sarah’s sweat or Priya’s frustration? Start by acknowledging you’re not broken—it’s not “all in your head.” Menopause symptoms are real, backed by data that’s finally catching up to the lived reality.
Track your symptoms in a journal; apps like Menopause Tracker make it easy to spot patterns and share them with your doctor. Talk openly—with friends, doctors, even your boss. Workplace policies are evolving, with 15% of U.S. companies in 2025 offering menopause-specific benefits like telehealth or flexible schedules. And don’t shy away from small tweaks: Swap coffee for herbal tea to ease flashes, or try a quick breathing exercise when anxiety spikes. Most importantly, connect with others—whether through a local group like Lisa’s or online communities where women trade stories and strategies.
The transition averages seven to 14 years, but most symptoms ease post-menopause. By shining a light on the hidden toll, you reclaim your narrative. Menopause isn’t the end of anything—it’s the bold beginning of a wiser, fiercer chapter. So, take a deep breath, grab that journal, and step into this phase with the strength you’ve always had. You’re not alone, and you’re far from powerless.
https://www.who.int/news-room/fact-sheets/detail/menopause